Pediatric calls are among the most challenging and emotionally charged situations that EMS professionals face. Children make up a significant portion of EMS patients, with studies showing that they account for approximately 5-10% of all EMS calls [1]. These emergencies can range from respiratory distress and febrile seizures to traumatic injuries and sudden infant death syndrome (SIDS).
 One of the primary challenges in treating pediatric patients is their anatomical and physiological differences compared to adults. Children have smaller airways, less blood volume, and immature immune systems, making them more vulnerable to certain conditions [2]. EMS providers must be well-versed in pediatric-specific assessment techniques, medication dosing, and equipment sizes to provide appropriate care.
One of the primary challenges in treating pediatric patients is their anatomical and physiological differences compared to adults. Children have smaller airways, less blood volume, and immature immune systems, making them more vulnerable to certain conditions [2]. EMS providers must be well-versed in pediatric-specific assessment techniques, medication dosing, and equipment sizes to provide appropriate care.
Rapid response and treatment are crucial in pediatric emergencies. This highlights the importance of EMS providers being prepared to quickly identify and manage life-threatening conditions in children.
Another aspect of pediatric calls that EMS professionals must navigate is the emotional impact on both the child and their family. Children may be frightened by the presence of strangers in uniform and the unfamiliar medical equipment. EMS providers must be skilled in communicating with children in an age-appropriate manner and providing reassurance to help alleviate their anxiety.
Furthermore, the presence of distraught parents or caregivers can add an additional layer of complexity to pediatric calls. EMS professionals must be able to effectively communicate with family members, explaining the child’s condition and the treatment being provided while also managing their emotional distress. A study in the Journal of Emergency Medicine found that clear, empathetic communication by EMS providers can help reduce parental anxiety and improve overall satisfaction with the care received [4].
Pediatric calls are a stark reminder of the fragility of life and the immense responsibility that EMS professionals bear. They require a unique blend of medical expertise, emotional intelligence, and the ability to remain calm under pressure. By staying up-to-date with the latest pediatric emergency care guidelines and continually honing their skills, EMS providers can make a profound difference in the lives of their littlest patients and the families who love them.
🚑 Be Better At EMS 🚑
Sources:
[1] Shah, M. N., Cushman, J. T., Davis, C. O., Bazarian, J. J., Auinger, P., & Friedman, B. (2008). The epidemiology of emergency medical services use by children: an analysis of the National Hospital Ambulatory Medical Care Survey. Prehospital Emergency Care, 12(3), 269-276. [URL]
[2] Anatomical and Physiological Differences in Children. (n.d.). Retrieved from [URL]
[4] Ayub, E. M., Sampayo, E. M., Shah, M. I., & Doughty, C. B. (2017). Prehospital providers’ perceptions on providing patient and family centered care. Prehospital Emergency Care, 21(2), 233-241. [URL]
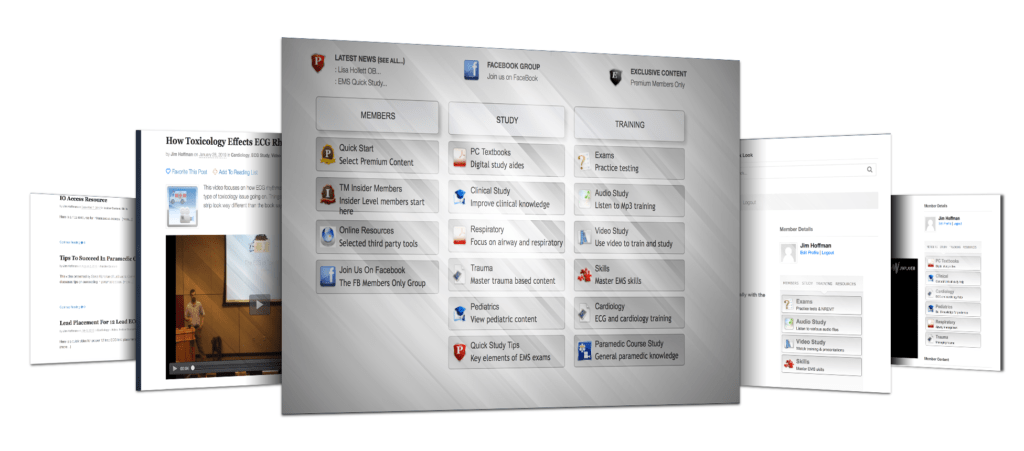
It's True. Over 900 EMT's & Paramedics are using Turbo Medic to finally see...
How To Pass Exams & Succeed In EMS. Even if they have struggled before on exams like the NREMT.
“Get a variety of study and review resources to help you pass exams, master content and be better at EMS”